Medical Billing & Coding Audit Services
Stay Aligned with Your
Payers and Patients!
You dedicate yourself to delivering quality care—but are you receiving the compensation you deserve? Billing errors can lead to lost revenue, denied claims, and even legal issues. That’s why medical billing audit services from a trusted medical coding audit company are essential.
NSMD provides expert healthcare coding and compliance audit services tailored for providers. Our experienced auditors review your billing codes for accuracy, compliance, and optimization, offering real-time issue resolution. Don’t leave your practice vulnerable—contact us today and ensure your billing meets regulatory standards.
Book A Free Consultation

What is a Medical Billing Audit?
Medical billing and coding audits serve as essential checkups to ensure that a provider’s claims and documentation comply with medical billing standards. Certified billing auditors review patient charts and billing records to verify the accurate use of codes that reflect the patient’s condition and the care provided. Much like routine physicals help detect health issues early, audits identify billing problems so providers can make timely corrections.
These audits are crucial because they uncover issues such as incorrect coding, incomplete documentation, missed charges, and noncompliance with reimbursement policies. By addressing these problems proactively, providers can strengthen their revenue cycle, reduce denied claims, and avoid penalties. Regular, thorough audits support accurate coding, complete records, proper reimbursement, payer compliance, and the overall financial well-being of a practice.
How does NSMD Support You as a Medical Coding Audit Company?
NSMD operates as a trusted provider of professional medical billing audit services. Given the complexity of medical billing and coding—where errors can easily occur—our audit and compliance solutions act as a safeguard, maintaining the integrity of the entire medical claims process.
Our experienced billing auditors closely examine documentation, coding decisions, and submitted claims to detect inaccuracies and highlight areas for improvement in the billing cycle. These insights guide healthcare providers toward precise coding and complete revenue capture.
Equally important, our high-quality audit program helps prevent compliance violations and potential fraud that could result in fines, penalties, or reputational harm. NSMD’s audit services form a critical foundation for achieving clinical accuracy, financial strength, and regulatory compliance.
Explore Our Medical Billing Audit Solutions
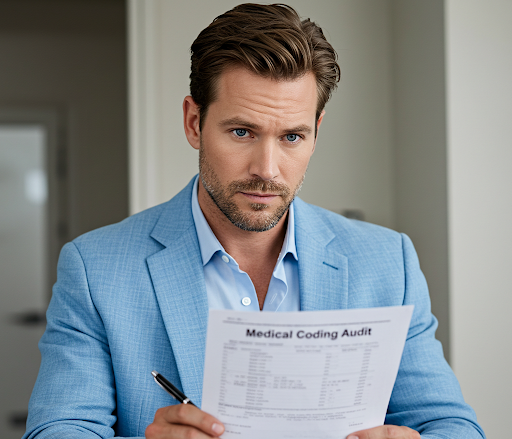
Medical Coding Audit
Medical Coding Audit

Medical Billing Audit
Medical Billing Audit
Government & Payor Mandated Audit
Government & Payor Mandated Audit

Clinical Audits
Clinical Audits

Collection Aging Audit
Collection Aging Audit

Auditing Medicare Patient Charts
Auditing Medicare Patient Charts
Are you unsure about the quality of your medical records?
Let us help you clarify them!
Your Billing Issues and Our Auditing Solutions
Inaccurate billing and coding practices can be costly for medical practices. Denied claims result in lost revenue, backlogs cause cash flow issues, and errors lead to audits and penalties. Our medical billing and coding audit service identifies the flaws in your workflows. After thoroughly analyzing your people, processes, and technology, we provide targeted recommendations to ensure compliance and optimize your revenue cycle.
Billing Inaccuracies
Impact the financial health, cash flow, profitability, and long-term viability of healthcare organizations.
Accurate Billing Claims
Through our comprehensive billing audit, we meticulously review each claim for accuracy, ensuring maximum appropriate reimbursement and supporting the financial health and longevity of your healthcare organization.
Coding Errors
Result in claim denials, revenue loss, overcharges, underpayments, patient dissatisfaction, and potential legal issues.
Over 99% Claim Acceptance
We use advanced NLP and machine learning techniques to analyze medical records, identify coding errors, optimize reimbursement, and prevent claim denials in the future.
Compliance Issues
Lead to penalties, fines, audits, investigations, lawsuits, sanctions, and exclusion from federal healthcare programs.
Achieve Billing Compliance
Our advanced billing analytics engine detects trends, outliers, and red flags in real-time, enabling targeted audits to address compliance risks and prevent government scrutiny.
Reimbursement Reductions
Could compel healthcare providers to reduce staff, limit services, close practices, or accept fewer Medicare patients.
Optimal Reimbursements
Our proprietary AI-driven billing audit system analyzes your claims data to uncover missed revenue opportunities and compliance risks, ensuring every dollar is captured before reimbursement cuts impact your bottom line.
We Optimize Your Medical Billing and Coding Systems
Internal Audit
Internal Audit
External Audit
External Audit
Prospective Audit
Prospective Audit
Retrospective Audit
Retrospective Audit
Comprehensive Audit
Comprehensive Audit
Missing Money? We'll Find It.
Missing Money? We'll Find It.
NSMD Latest Auditing Solutions
Our Coding Audit Service Guarantees Billing Compliance: We Achieve This By:

Auditing the accuracy of your coding
Assessing coding accuracy is a core objective of our medical coding audit service. We conduct thorough investigations of medical charts to ensure that codes align with the diagnosis, procedures performed, and complexity of care. Accurate coding is essential for proper reimbursement and compliance with guidelines. Our audits detect issues like upcoding or undercoding and provide recommendations for corrective actions. With our support, healthcare providers can be confident that their coding practices meet standards and fully capture the value they are entitled to.
Auditing the accuracy of your charge capture
Another key area we focus on is charge capture. We ensure that all services provided and supplies used are accurately reflected in the billing at the correct rates. Missed charges result in lost revenue, so we carefully compare the medical record documentation to the itemized billing statement. Any missed charges are identified, and we suggest improvements to the charge capture process. Our aim is to maximize your reimbursement by addressing gaps where valid charges may have been overlooked.

Auditing your billing documentation for compliance
A comprehensive documentation review is also included in our billing audit process. We evaluate whether the medical record contains clear, consistent documentation that supports the coded claims. Complete and accurate documentation is essential for justifying charges and withstanding payer scrutiny. Our team identifies any documentation issues such as ambiguity, inconsistency, missing signatures or credentials, or insufficient medical necessity. We offer recommendations to improve documentation practices, ensuring stronger claim defense and better preparedness for audits.

Auditing provider-payer contracts for compliance and accuracy
We also audit the proper application of insurance payer contracts and fee schedules, as well as the accuracy of data entered into the billing system. Incorrect fee schedules and data entry errors can jeopardize reimbursement. We ensure compliance with payer contracts and suggest process improvements to enhance billing system accuracy. Our comprehensive audits cover all critical areas to maximize claim quality and maintain revenue integrity.
Our Coding Audit Services Ensure Billing Compliance:
This Is How We Do It
Receive Post-Audit Reports Directly in Your Inbox
Receive Post-Audit Reports Directly in Your Inbox
Charge Capture Evaluation Report
Charge Capture Evaluation Report
Coding Accuracy Audit Report
Coding Accuracy Audit Report
Claim Denial Review Report
Claim Denial Review Report
Compliance Risk Evaluation Report
Compliance Risk Evaluation Report
Charge Capture Assessment Report
Charge Capture Assessment Report
Elevate Your Data Accuracy and Regulatory Compliance
Medical Chart Audits and Validations
NSMD’s team of certified doctors, auditors, and clinicians can conduct a variety of medical chart reviews, including:
Medical Chart Evaluations
Our clinical auditors conduct comprehensive medical chart reviews, including inpatient, outpatient, radiology, DME audits, mammography audits, and more. These reviews evaluate the quality of care delivered, ensure compliance with coding and documentation standards, and verify adherence to established clinical guidelines.
Risk Data Verification
We can validate the accuracy of your risk adjustment data, including diagnosis codes, hierarchical condition categories (HCCs), and risk scores. This ensures optimized reimbursement, helps avoid penalties, and enhances patient outcomes.
Data Abstraction Assessment
We extract and abstract key data from your medical charts, including diagnoses, procedures, medications, lab results, and quality measures. Additionally, we verify the accuracy of data entry in your EHR or other systems.
Charge Verification
We assess your charge capture process to ensure that the charges billed to payers are accurate and supported by the documentation in the medical chart. Additionally, we identify and address any undercharges or overcharges that could impact your revenue cycle.
Are your claim submissions error-free and compliant?
Allow us to conduct a free health check for your practice.




